
Disease Pathology
The Human Eye
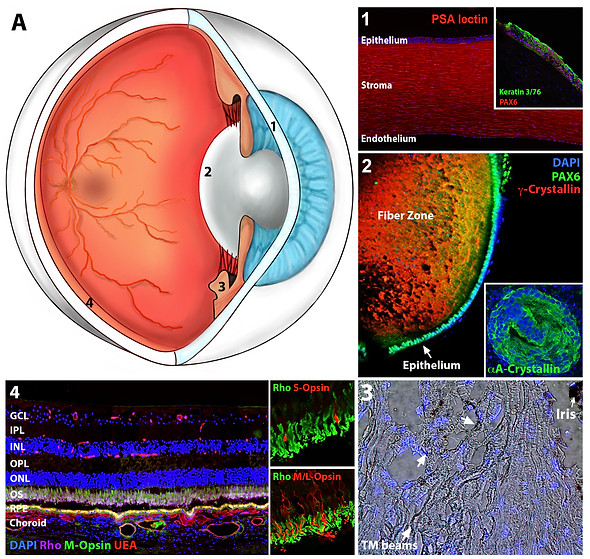
The human eye (panel A) is a complex organ that is made up of several different structures.
On the most basic level, the eye can be subdivided into two main portions.
1) The anterior chamber, which contains the cornea (panels A1 & 1), the lens (panels A2 & 2) and the trabecular meshwork (panels A3 & 3).
2) The posterior chamber, which contains the neural retina, underlying RPE cell layer and deeper choroidal vasculature (panels A4 & 4).
The structures of the anterior chamber are largely responsible for focusing light, reflected from surfaces in our environment, onto the retina. The retina in turn is responsible for turning this light into electrical signals that are sent to the brain via the optic nerve. These patterns of light are in turn interpreted by the brain as coherent perceptions of the world around us.
The Retina

The neural retina is a multilayered tissue that covers the posterior pole of the eye. The innermost layers (GCL and NFL) contain retinal ganglion cells and their axons, which make up the optic nerve. The inner nuclear layer (INL) contains the cell bodies of 4 distinct cell types, namely bipolar cells, amacrine cells, horizontal cells and muller glial cells. The outer nuclear layer contains the light sensing photoreceptor cells. Beneath are the retinal pigment epithelial (RPE) and choroidal endothelial cells (CEC) within the RPE layer and choroid respectively.
As light enters the eye it passes through the inner layers of the retina before being detected by photoreceptor cells and converted into an electrical signal and sent to the brain via the optic nerve.
While dysfunction of anterior chamber tissues can result in significant vision loss, in the developed world diseases associated with these tissues are largely treatable via drug and/or surgical intervention. For instance, cataracts, which are a leading cause of blindness in under developed regions of the world, are routinely treated via lens replacement in developed countries.
While invaluable drug and surgical interventions have been developed for the treatment of disorders that affect the retina, they are largely designed to prevent cell death. Death of light sensing photoreceptor cells, which is associated with diseases such as age related macular degeneration (AMD) and retinitis pigmentosa (RP), is the leading causing of irreversible blindness in the developed world.
Inherited retinal degeneration

Mutations in any one of more than 100 different genes have been shown to cause photoreceptor cell death.
Our understanding of inherited retinal disease has benefited immensely from molecular genetic analysis over the past several decades. New technologies that allow for increasingly detailed examination of a patient's DNA have expanded the catalog of genes and specific variants that cause retinal disease.
The identification of pathogenic variants has allowed for the development of gene therapies and autologous cell therapies. Despite this progress, a relatively large fraction (i.e., at least 20%) of patients with clinical features suggestive of an inherited retinal disease still do not have a molecular diagnosis today. Variants that are not obviously disruptive to the codon sequence of proteins can be difficult to distinguish from the background of benign human genetic variations.
Verification of Variant Pathogenicity

B) Transcription or transcript processing (e.g. cryptic splice variants, variants impacting gene expression regulation). C) Synaptic formation or function. D) Connecting cilia. E) Disc morphogenesis. F) Lysosomal storage. G) Protein folding or proteasomal degradation. H) Translation or ribosomal function. I) ER-stress. J) Mitochondrial function.
